Helping Healthcare Organizations with RCM Services,
Analytics, and Custom Software Development
We deliver intelligent, end-to-end solutions for revenue optimization, data-driven decision-making, and tailored software—built to meet the unique needs of modern healthcare organizations.
Revenue Cycle Management
Team Augmentation Outcome-Based
Healthcare Analytics
Custom Reporting Data Analysis
Custom EMR/EHR Development
Scheduling Patient Portal
Our Services
As your trusted partner, we provide staff for revenue cycle management through team augmentation and outcome-based models, alongside custom reports, dashboards, and data insights. We also deliver scalable software development solutions to optimize revenue and accelerate growth.

RCM Services
Streamline operations, improve cash flows, and reduce administrative burden with our skilled RCM team.

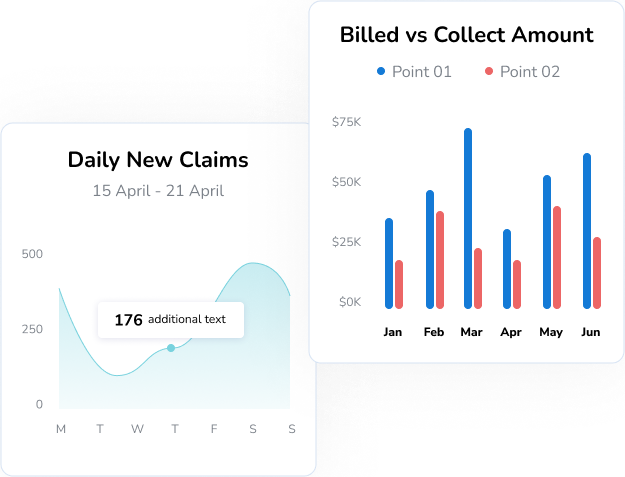
Healthcare Analytics
Transform your data into actionable insights. We help you build scalable analytics platforms that boost decision-making and user satisfaction.

EMR/EHR Development
From concept to deployment, we create tailored software and applications that are secure, responsive, and built for performance across all platforms.
RCM Solutions
Our skilled team streamlines your entire revenue cycle—from billing and claims to payments—helping you reduce errors, save time, and boost profitability.
Streamline your billing process and ensure faster reimbursements with accurate, compliant claim handling.
- Clean and timely claim submission
- Payment posting and reconciliation
- Rejection management and resubmissions
- Real-time billing status tracking
- Customized financial reporting
Ensure accurate, compliant, and timely coding to improve claim approvals and reduce denials.
- ICD-10, CPT, and HCPCS coding expertise
- Specialty-specific coding for all medical fields
- Error-free documentation and code audits
- Support for inpatient and outpatient services
Improve cash flow and reduce aging with proactive, end-to-end accounts receivable management.
- Real-time tracking of outstanding claims
- Timely follow-ups on unpaid or underpaid claims
- Automated alerts for aging accounts
- Root cause analysis of payment delays
- Comprehensive AR performance reports
Ensure your providers are enrolled, verified, and ready to deliver care without delays or denials.
- End-to-end provider enrollment management
- Payer applications and revalidations
- Primary source verification
- Compliance with regulatory standards
- Ongoing credential tracking and updates
Reduce revenue loss by identifying, analyzing, and resolving claim denials quickly and effectively.
- Root cause analysis of denials
- Corrective resubmissions and appeals
- Denial trend tracking and reporting
- Payer-specific denial resolution
- Workflow optimization to prevent future denials
Prevent claim denials and delays by confirming patient coverage before services are rendered.
- Real-time insurance eligibility checks
- Verification of benefits, copays, and deductibles
- Automated payer communication
- Reduced claim rejections due to ineligibility
- Seamless integration with scheduling and billing
Who we Serve
We partner with clinics, hospitals, billing companies, and healthcare startups to build custom software that improves operations, enhances care delivery, and drives smarter, more efficient revenue cycle management.
#1
Hospitals & Health
Systems
#2
Private Clinics &
Practices
#3
Medical Billing &
RCM Companies
#4
Healthcare Startups
& Tech Firms
#5
Telemedicine & Virtual
Care Providers
We Work with All Types of Healthcare Analytics
As your healthcare technology partner, Axascale empowers better decisions through advanced analytics. From insights to actions, we help you improve care delivery, streamline operations, and boost revenue outcomes.
1. Descriptive Analytics
We analyze historical healthcare data to clearly explain what happened over a period of time.
e.g. Average ER wait time, billing trend tracking, peak hour identification.
2. Diagnostic Analytics
We examine patterns and relationships in your data to uncover why something happened.
e.g. No-show pattern analysis, claim denial reasons, delay investigation.
3. Predictive Analytics
We use AI/ML models to forecast what is likely to happen next, helping you stay proactive.
e.g. Patient inflow forecast, high-risk claim prediction, seasonal trend analysis.
4. Prescriptive Analytics
We recommend specific actions based on data insights to determine what should be done.
e.g. Staff schedule optimization, follow-up prioritizations, claim automation suggestion.
Custom EMR/EHR Solutions
A flexible, end-to-end EMR/EHR solution built to fit your workflows—simplifying patient care, documentation, and compliance while improving provider efficiency.
- Patients Management
- Appointment Scheduling
- Patient Revaluation
- Bill Generation
- Document Management
- Denial Management
- Payment Management
Patient / Case Management
We can build custom softwares for healthcare teams to manage patient records, demographics, medical histories, and ongoing cases from a single, secure interface. Whether it’s a first-time visit or long-term care, everything is organized for faster access and smarter care delivery.
Key Features
- Complete patient profiles with demographic and medical history
- Link appointments, documents, billing, and communications
- Track active, recurring, or discharged cases
- Role-based access for providers, admins, and support staff
- Case timeline for a holistic view of the patient journey
Appointment scheduling ensuring availability of doctors and practice timings
We can build smart appointment scheduling systems that aligns with your provider availability, clinic hours, and specialty needs. Easily manage slots, avoid double bookings, and optimize your daily workflow with automated reminders and rescheduling options.
Key Features
- Real-time provider availability tracking
- Custom time slots and recurring appointments
- Automated patient reminders (SMS/email)
- Integrated with calendars and front desk workflows
- Supports walk-ins, cancellations, and reschedules
Patient Revaluation by Providers
Efficient assessments for informed clinical care.
Our system enables providers to perform, track, and review patient evaluations with ease. From initial consults to follow-ups, you can document findings, compare health trends, and ensure accurate, real-time access to patient data—all within a unified platform.
Key Features
- Customizable evaluation templates (e.g., SOAP notes, specialty forms)
- Integrated vitals and clinical history
- Visual progress tracking (e.g., lab results, symptom changes)
- Easy comparison with past assessments
- Support for multi-provider input
Bill / Invoice Generation
Fast, accurate, and fully integrated billing.
Our system simplifies medical billing by automating invoice creation based on treatments, procedures, and insurance rules. From patient visits to insurance claims, every bill is generated with precision and connected to your broader revenue cycle—minimizing errors and speeding up reimbursements.
Key Features
- Auto-generated invoices from visit data
- Custom billing templates (e.g., by specialty or payer)
- Insurance and self-pay support
- ICD-10/CPT code integration
- Real-time billing status tracking
Document Management
Secure, organized, and easily accessible records.
Our system provides a centralized and secure space to store, manage, and retrieve all clinical and administrative documents. From scanned referrals to diagnostic reports, everything is linked to the right patient and instantly accessible—streamlining workflows and supporting compliance.
Key Features
- Centralized document storage by patient/case
- Uploads for labs, referrals, and scanned files
- Role-based access and permissions
- Easy search and retrieval
- HIPAA-compliant security protocols
Denial & Verification Management
Proactive control over claim approvals and denials.
Our system helps you manage insurance verifications and claim denials with speed and accuracy. From verifying patient eligibility to tracking denial reasons and resubmitting claims, we ensure every step of the process is streamlined and optimized for faster reimbursements.
Key Features
- Real-time insurance eligibility checks
- Denial tracking with categorized reasons
- Resubmission workflows and status updates
- Alerts for missing or incorrect information
- Integration with billing and coding modules
Payment Management
Simplified tracking of patient and insurance payments.
Our system ensures complete visibility into all financial transactions—from patient co-pays to insurance reimbursements. You can track, allocate, and reconcile payments in real-time, while improving transparency for both your team and your patients.
Key Features
- Real-time payment posting and tracking
- Split payments and partial collections
- Automated receipts and payment history
- Integration with billing and denial workflows
- Patient payment portals and reminders
TESTIMONIALS
What Our
Clients Say

“Axascale completely transformed our billing workflow. What used to take hours now takes minutes, and the accuracy is unmatched. Their team really understands healthcare operations.”
Daniel Roberts
Co-Founder
“From appointment scheduling to payment tracking, everything is now streamlined. The EMR/EHR solution they built for us fits our practice like a glove.”
James Gold
Co-Founder
“Their analytics platform has given us insights we didn’t know we needed. We can now make informed decisions faster and deliver better patient care.”
Harvey Leon
Operations ManagerTestimonials
What our Clients Says






